One of the best decisions you can ever make when dealing with the impact of a chronic disease diagnosis is getting as much mental health support as possible.
If you have ever been diagnosed before, you will understand how important and far-reaching this can be in helping you manage your condition.
It is challenging to deal with the daily battles, the unending uncertainty, and the emotional toll it takes—it can be exceedingly overwhelming.
Hence, it is crucial to consider getting therapy for chronic illness management. It’s not just about sitting down and talking with a stranger; it’s about discovering incredible ways to regain control, resilience, and a better quality of life.
Impact of chronic illness on a person
Being diagnosed with a chronic illness significantly impacts a person’s life. This impact ranges from physical to psychological or mental.
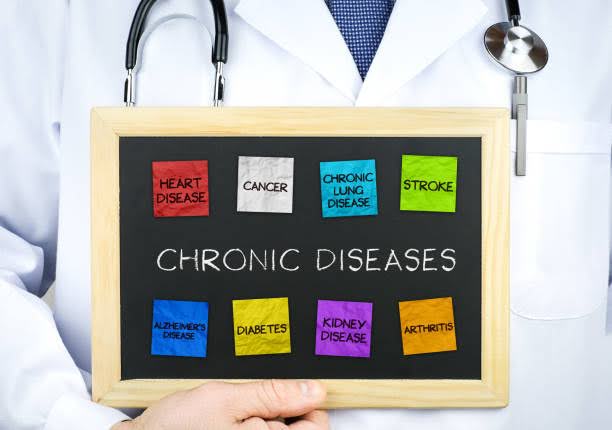
Here’s a breakdown of these impacts:
1. Physical impact of chronic diseases
The physical impact of a chronic illness depends on the type of illness, its severity, and how well it is managed, and it can include:
Pain
Many chronic illnesses, like fibromyalgia, endometriosis, rheumatoid arthritis, and so on, cause intense pain. The severity of the pain can make it difficult to sleep, eat, and participate in physical activities.
Disability
Some chronic illnesses like arthritis, stroke, and epilepsy can lead to disabilities. This can cause a lot of limitations in movement and basic activities due to difficulties with walking, standing, or performing daily activities.
Sleep problems
Sleep and chronic disease are connected in several ways, as several people diagnosed with chronic diseases develop sleep disorders. Getting a good night’s sleep becomes difficult, worsening other symptoms.
Dietary restrictions
Some chronic illnesses require strict dietary restrictions. For instance, people with celiac disease must avoid foods that contain gluten, while those with severe food allergies have to be picky with the food they eat to prevent any allergic reactions.
Physical changes
Certain chronic illnesses can affect a person’s physical appearance. For example, skin conditions like psoriasis, hair loss from alopecia, or the visible symptoms of lupus can lead to self-esteem issues and social challenges.
Reduced lifespan
Some chronic illnesses can shorten a person’s lifespan. It can be a complicated reality to face, but it is important to focus on living the best life possible with the time that one has.
RELATED POSTS:
2. Emotional and psychological impact of chronic diseases
The emotional and psychological impact of chronic diseases concerns how the illness affects your feelings and the emotional responses you experience. It also shows how chronic illness diagnosis and management affect your mental health.
Here are some of the emotional and psychological effects of chronic diseases:
Stress and Anxiety
Dealing with a chronic illness can be highly stressful. You may worry about your symptoms, treatment options, financial burdens, and how the illness will affect your future. It can increase your anxiety levels and even result in panic attacks and other anxiety disorders.
Depression
Chronic illnesses are often linked to an increased risk of depression. The condition’s nature, physical limitations, and lifestyle changes can cause feelings of hopelessness, sadness, and depression.
Social Isolation
Managing a chronic illness can result in social isolation. You may withdraw from social activities due to physical limitations, fear of judgment, or insecurity.
Low Self-Esteem
Physical changes or limitations caused by chronic illnesses can negatively impact your self-esteem and self-worth. You may also struggle with body image issues and feel like you are a burden to others, especially if you need to rely on others.
Negative Coping Mechanisms
People with chronic illnesses may develop both healthy and unhealthy coping mechanisms. However, negative coping mechanisms don’t take much work, and they are easy to develop, including unhealthy habits like overeating, substance abuse, or avoidance behaviors to deal with emotional distress.
Reduced Adherence to Treatment
The psychological impact of a chronic illness can affect your motivation and ability to adhere to prescribed treatments and medications, leading to poor disease management.
The mental responses of a person to chronic illness can vary. Some people develop coping strategies themselves, while others might need the help of a professional therapist to overcome the effects.
How getting therapy for chronic illness helps you
Getting therapy for chronic illness is one of the best ways to manage your health.

There are several impacts of chronic illness on a person’s life, and the most dangerous impact is the mental health impact because a person might be suffering internally without having anyone to open up to.
However, getting therapy can help you manage the mental health effects of your condition.
Here are the ways that getting therapy for chronic diseases helps:
1. Coping with the emotional and mental effects of chronic illness
Getting therapy for a chronic illness can be immensely beneficial in helping you cope with the emotional and mental effects associated with it.
Therapy provides a supportive environment where you can openly discuss your feelings and the struggles related to your condition.
A therapist can also help you develop practical and positive coping strategies to manage stress, anxiety, depression, and other mental health effects of your diagnosis, as well as provide guidance in understanding and accepting the changes and limitations of chronic illness.
With good therapy, you can improve your self-esteem, address any trauma or emotional distress you may have experienced, and enhance your motivation and medication adherence.
2. Improving quality of life
Your quality of life can improve when you get therapy for a chronic illness. Therapy provides you with the essential emotional support you need. This support allows you to show your vulnerabilities, fears, and weaknesses without being judged.
Because of this, you can express yourself, which ultimately reduces stress and anxiety.
You will also come to terms with your condition and make necessary adjustments. Through therapy, you can better understand your illness and learn ways to manage it effectively.
Your relationships with your family and friends can also benefit from therapy. Therapy allows you to express yourself, making communicating with your family easy. You can learn how to set boundaries with your family members and how you can teach them to help you.
When your self-confidence is boosted, and you have improved communication with your family, it becomes easier for you to maintain a good quality of life.
3. Adhering to treatment
Therapy for chronic illnesses can play a vital role in improving your medication and treatment adherence.
Firstly, therapy provides a safe space for you to discuss any concerns or reservations about your treatment plan. You can quell doubts, overcome obstacles, and gain clarity and understanding through open and honest conversations with your therapist.
You can also identify and overcome barriers to medication adherence, like forgetfulness and trauma. Doing this can help increase your medication’s effectiveness and work toward realistic treatment goals.
Personalized and even general therapy sessions can help to improve your overall self-efficacy—the belief in your ability to manage your condition and adhere to your treatment. A therapist can help you build self-confidence to push you toward positive self-advocacy and medication adherence.
4. Improving self-management
Seeking therapy for chronic illness can enhance your ability to self-manage your condition. Therapy offers a valuable and accepting space for you to understand your illness better.
It is much better when you are part of a chronic illness support group; this fosters understanding and acceptance. The mere fact that you are not alone can push you to become actively involved in your disease management.
Your therapist can also help you comprehend the nature of your condition, its triggers, and how it affects your body, which is crucial for chronic illness management.
You can develop personalized self-management plans with your therapist, including medication adherence, dietary modifications, exercise routines, and stress reduction techniques. These bite-sized, personalized plans will empower you with the skills and knowledge you need to take control of your health.
Your therapist can offer guidance and support as you work toward these objectives, ensuring you stay on course.
Living with a chronic illness can be unpredictable, and there may be times when your symptoms worsen or you experience sudden flares that frustrate you and make you tired. However, you can build the resilience needed to bounce back from these setbacks with therapy.
5. Motivation
Motivation often goes hand in hand with acceptance in therapy.
You gain motivation by learning how to accept yourself with the help of a professional therapist. A support system or a chronic illness support group can also help you understand that you are not alone.
A therapist can help you identify your reasons for not adhering to your treatment plan and making the necessary lifestyle changes for optimal health.
By exploring your intrinsic motivations, you can understand yourself and strengthen your commitment to self-care.
Your therapist can also assist you in setting achievable goals and tracking your progress, providing you with a tangible sense of accomplishment and motivation.
In therapy, you can learn to address and overcome emotional barriers, ultimately boosting your motivation to manage your condition actively. Through therapy, you develop the mental fortitude to stay motivated and persistent in your self-management efforts, even when faced with challenges.
Common barriers to therapy for chronic illnesses
Many individuals with chronic illnesses face several common barriers that hinder them from seeking therapy to address their emotional and mental health needs. These barriers include:
Stigma
The stigma surrounding mental health issues can prevent people from seeking therapy for chronic illnesses, coupled with the fear of judgment and stigmatization.
High cost of therapy sessions
The cost of therapy sessions can be a significant barrier, especially when you don’t have health insurance coverage for mental health services.
Limited availability of specialized professionals
Finding a therapist or mental health professional with expertise in chronic illness and mental health can be challenging.
Scheduling conflicts with work
Balancing therapy sessions with work commitments is also a common barrier. You may hesitate to take time off work to attend therapy appointments even if you are self-employed.
Lack of knowledge about therapy benefits
Not understanding how beneficial therapy is for managing the emotional and mental aspects of chronic illness can pose a barrier. It can deter you from seeking help.
Fear of privacy and confidentiality breaches
Privacy and confidentiality concerns are another barrier to seeking therapy. The constant worry that your personal health information and mental health struggles could be disclosed without your consent can lead to reluctance to seek therapy.
CONCLUSION
Your journey toward a brighter, more fulfilling future begins with the decision to seek therapy—a decision that empowers you to live your best life, chronic illness and all.
As you reflect on the amazing ways therapy for chronic illness can transform your life, remember that good things take time. It might be hard to open up initially, so take your time.
Do you get therapy as part of your chronic disease management techniques? How has it helped you so far?
READ ALSO: 9 Vitals Things to Check in Chronic Illness Support Groups



0 Comments